Carcinoma Esophagus
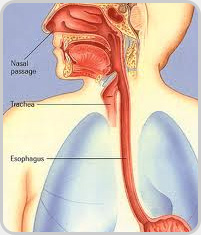
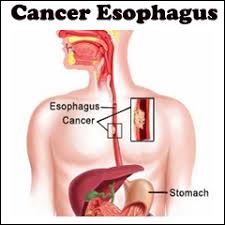 The esophagus is a muscular tube also known as food pipe in general public transmits food material from mouth (base of pharynx) to the stomach. Cancers of esophagus is one of the deadliest malignancies of human body. The incidence of this malignancy is increasing in general population due to poor life style as well as changes in environment.
The esophagus is a muscular tube also known as food pipe in general public transmits food material from mouth (base of pharynx) to the stomach. Cancers of esophagus is one of the deadliest malignancies of human body. The incidence of this malignancy is increasing in general population due to poor life style as well as changes in environment.
Carcinoma of esophagus is divided into two types -
Risk factors for Esophageal malignancy -
Diagnosis of esophageal malignancy
The patient is evaluated on the basis of history, symptoms and clinical signs. Along with routine blood test and X-ray some endoscopic and radiological investigations are done which include -
Patients with esophageal cancer are managed based on its stage. Overall general condition of the patients affects management.
Stage I -
Tis and T1aN0 stage -
Endoscopic therapy like mucosal resection or submucosal dissection with the help of endoscopic ultrasound (EUS)
Photodynamic therapy
Radiofrequency ablation
T1b N0 & T2 N0 stage - Surgery (esophagectomy) to remove the part/whole of esophagus that contains the cancer.
Stages II-III - Chemoradiation followed by surgery (trimodal therapy)
Patient with squamous cell carcinoma with well preserved general condition chemotherapy and radiotherapy started to downstage the tumor before definitive surgery.
Patients with adenocarcinoma of lower end esophagus where stomach meet (gastroesophageal junction) are given chemotherapy or chemoradiation before surgery.
Patients with serious co-morbidities who are not candidate for surgery are managed with radical chemoradiation with curative intension.
Stage IV - Chemotherapy/Radiotherapy or symptomatic and supportive care Treatment is given only for palliation to relieve the symptoms like pain, difficulties in swallowing etc.
Esophageal stenting (plastic/metallic) is done in situations where the patient cannot swallow at all and having Tracheo/broncheo esophageal fistula (communication between food pipe and wind pipe.
Patient who are unable to tolerate oral feeds a nasogastric tube may be required to continue feeding.
Some times gastrostomy/jejunostomy tube is required where patients become intolerant to nasogastric tube or tend to aspirate food.
Laser therapy is done in cases in which esophagus is totally occluded by cancer and the cancer cannot be removed by surgery. The relief of a blockage by laser can help to reduce dysphagia and pain. The therapy is less often used.
Chemotherapy:Chemotherapy may be given after surgery (adjuvant) to reduce risk of recurrence or before surgery (neoadjuvant) to down stage the disease.

Radiotherapy is given before, during or after chemotherapy or surgery. It is also used in palliation to control pain.
Surgery is contraindications in following situation:
Surgical options: - Surgery is performed by either open or minimal invasive method depending upon patient's general condition and availability of experts. Now a days minimal invasive approach of esophagectomy has become very popular among surgeons because of low surgical morbidity, short hospital stay and similar oncological outcomes.
(1) Minimal Invasive Esophagectomy (MIE) – Minimal invasive Esophagectomy is done by Thoracoscopic and laproscopic methods (key hole surgery). The esophgus is removed with slander instrument from key hole under guidance of camera and monitor. The oncological results are similar to open methods but early recovery and less ICU stay and lest chest complications are seen with MIE. The minimal Invasive esophagectomy can also be performed with Robotic assistance which also has the same advantages of thoracoscopy . The current evidence does not support the superiority of robotic surgery, prticularly in view of high cost involed.
In Thoracoabdominal Approach –both the abdominal and thoracic cavities opened together.
Ivor Lewis Esophagectomy –two-stage approach involves an initial laparotomy and construction of a gastric tube, followed by a right thoracotomy to excise the tumor and create an esophagogastric anatomises in chest.
McKeown Esophagectomy –Three-stage approach which include incision in the neck to complete the cervical anastomosis in neck.