Neuroendocrine Neoplasm / Neuroendocrine Tumors
 Neuroendocrine Neoplasm (NENs) are tumors that arise from cells of the endocrine and nervous systems. Neuroendocrine cells make hormones that control digestive juices and the peristalsis used in moving food through the stomach and intestines. Digestive tract neuroendocrine tumors are slow growing rare tumors comprising less than 2 percent of gastrointestinal malignancies with location of the primary tumors in the lining of the gastrointestinal tract, most often in the stomach, appendix, small intestine, or rectum and pancreas, and biliary tract.
Neuroendocrine Neoplasm (NENs) are tumors that arise from cells of the endocrine and nervous systems. Neuroendocrine cells make hormones that control digestive juices and the peristalsis used in moving food through the stomach and intestines. Digestive tract neuroendocrine tumors are slow growing rare tumors comprising less than 2 percent of gastrointestinal malignancies with location of the primary tumors in the lining of the gastrointestinal tract, most often in the stomach, appendix, small intestine, or rectum and pancreas, and biliary tract.
NENs most often develop in the GIT or pancreas. These tumours are sometimes grouped together and called gastroenteropancreatic neuroendocrine Neoplasm (GEP NENs).
NENs of the gastrointestinal tract are most often arising from the lining of stomach, appendix, small bowel, and rectum. They are also called carcinoid tumours of gastrointestinal tract. Carcinoids most commonly affect the small bowel, particularly the ileum, and are the most common malignancy of the appendix.
NENs that develop in the pancreas are also called endocrine tumors of the pancreas.
These are all rare types of tumor and include -
Neuroendocrine tumors are divided into -
Risk factor
Most of the times cause of these NENs are not known.
Probable causes are-
Family history - multiple endocrine neoplasia type 1 (MEN1) syndrome, neurofibromatosis type 1 (NF1) syndrome, Von Hippel-Lindau syndrome (VHL) For gastric NETs - atrophic gastritis, pernicious anemia, Zollinger-Ellison disease
Symptoms and signs
 Majority of neuroendocrine tumors are non functional there by asymptomatic, or they produce symptoms related to the mass effect of the tumors. The symptoms are usually nonspecific and mimic a variety of diseases. They may be discovered incidentally during routine computerized tomographic examinations (CT-scan) of the abdomen for unexplained symptoms, or during removal of the appendix. Neuroendocrine tumors of pancreas can be classified into functional or non-functional tumors. Functional neuroendocrine tumors are associated with symptoms related to the secretion of specific hormones by the tumor such as hypoglycemia in patients with insulinoma, or hyperglycemia in patients with glucagonoma or somatostatinoma.
Non-functional neuroendocrine tumors, on the other hand, are associated with symptoms related to the mass effect of the tumors such as intestinal obstruction and abdominal pain.
Majority of neuroendocrine tumors are non functional there by asymptomatic, or they produce symptoms related to the mass effect of the tumors. The symptoms are usually nonspecific and mimic a variety of diseases. They may be discovered incidentally during routine computerized tomographic examinations (CT-scan) of the abdomen for unexplained symptoms, or during removal of the appendix. Neuroendocrine tumors of pancreas can be classified into functional or non-functional tumors. Functional neuroendocrine tumors are associated with symptoms related to the secretion of specific hormones by the tumor such as hypoglycemia in patients with insulinoma, or hyperglycemia in patients with glucagonoma or somatostatinoma.
Non-functional neuroendocrine tumors, on the other hand, are associated with symptoms related to the mass effect of the tumors such as intestinal obstruction and abdominal pain.
Symptoms of Neuroendocrine tumors may include the following:
Carcinoid syndrome -this may occur if the tumor has metastesized to the liver or other parts of the body and the liver cannot destroy the extra hormones made by the tumor, high amounts of these hormones may remain in the systemic circulation and cause carcinoid syndrome.
Symptoms of carcinoid syndrome include the following:
Diagnosis
Patient's medical history is evaluated in detail and a physical examination is done.
If a carcinoid tumor is suspected, blood and urine tests may be used to look for abnormal amounts of hormones and peptides produced by the tumor, including chromogranin A in blood and 5HIAA (a byproduct of serotonin) in the urine.
Newer markers -
Imaging tests - Ultrasound, CT-scans and MRIs may be performed to confirm the diagnosis, and to determine the exact location and size of the tumor, if it has spread to other organs, and whether it can be surgically removed
Triphasic CT Scanning - provides images during three different phases of blood flow through the liver, offer a more accurate diagnosis than routine CT. These tests are often used to determine whether the tumor has spread to the liver or nearby lymph nodes.
OctreoScan - Neuronedocrine tumours express somatostatin receptors providing a unique target for imaging. Octreotide is a synthetic modifications of somatostatin with a longer half-life., also called somatostatin receptor scintigraphy (SRS or SSRS), utilizes intravenously administered octreotide that is chemically bound to a radioactive substance, often indium-111, to detect larger lesions with tumor cells that are avid for octreotide.
Gallium-68 DOTANOC PET-CT - Somatostatin receptor imaging can now be performed with positron emission tomography (PET) which offers higher resolution, three-dimensional and more rapid imaging is much more accurate than an OctreoScan.
Fluorine-18 fluorodeoxyglucose (FDG) PET - This scan is performed by injected radioactive sugar intravenously. Tumors that grow more quickly use more sugar. Using this scan, the aggressiveness of the tumor can be visualized
MIBG Scintiscan - Some neuroendocrine tumors absorb the hormone norepinephrine. In this nuclear imaging technique involves giving patients an injection of MIBG, a protein similar to norepinephrine that is combined with a radioactive substance.
Radiation-sensitive imaging tests reveal how much MIBG has been absorbed, indicating the presence of a carcinoid tumor.
Upper Endoscopy : An endoscope is inserted through the mouth and passed through the esophagus into the stomach. Sometimes the endoscope also is passed from the stomach into the small intestine (Enteroscopy) to see the abnormal tissue growth. In case of obvious growth, biopsy is taken to confirm the diagnosis.
Colonoscopy : A colonoscope is inserted through the rectum into the colon to see abnormal growth. A biopsy from abnormal tissue is always taken to confirm the diagnosis.
Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An ultrasonic probe is attached at the end of the endoscope.
Capsule endoscopy : this is a noninvasive procedure to see all of the small intestine. The patient swallows a capsule that contains a tiny camera. As the capsule moves through the gastrointestinal tract, the camera takes pictures and sends them to a receiver worn on the outside of the body.
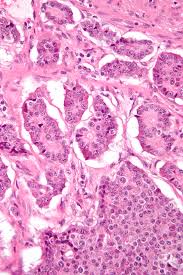
Biopsy : Tissue samples may be taken during endoscopy and colonoscopy from abnormal tissues. The biopsied tissues is viewed under a microscope to confirm the diagnosis. Sometimes further test like IHC are done on biopsy specimen to different different types of tumors.
Treatment : Treatments may be aimed at curing the disease or at relieving symptoms (palliation).
Localized tumors : Surgery is the primary treatment for localized tumors and might be curative. Surgical removal of the tumor is usually the first treatment for gastrointestinal carcinoid tumors. Tumors that have not spread may be removed along with a small portion of healthy tissue surrounding the tumor. Depending on the location of the tumor and whether it has spread, additional surgery may be required to remove portions of the affected organ or nearby lymph nodes.
Surgery can be done by either open or minimal invasive method (Laparoscopic or Robotic) to remove neuroendocrine tumors and nearby lymph nodes. In minimal invasive method, a laparoscope is inserted into the abdomen through a small incision. Benefits of minimal invasive method includes reduce postoperative pain, short hospital stay, less wound complications and faster recovery. Metastatic and recurrent disease.
In certain circumstances, complete removal of the tumor may not be possible. Role of surgery in metastatic disease is to reduce the tumor mass and can be performed before or concomitantly with medical treatment. Other means of cytoreductive procedures are available, such as radiofrequency ablation, laser therapy and embolization of liver metastases.
Cytotoxic treatment has been the standard for advanced neuroendocrine pancreatic tumors. The standard combination chemotherapy regimens include the following:
Biological treatment -
 Somatostatin analogues and a interferons has proved effective in control of associated clinical syndromes related to hormone production and release (carcinoid syndrome, gastrinoma, glucagonoma, etc.) in up to 60% of patients. Tumor-targeted radioactive treatment is an option in the selected group of patients with tumors that present a high grade of uptake of [111In] pentaoctreotide (octreoscan) scintigraphy.
Somatostatin analogues and a interferons has proved effective in control of associated clinical syndromes related to hormone production and release (carcinoid syndrome, gastrinoma, glucagonoma, etc.) in up to 60% of patients. Tumor-targeted radioactive treatment is an option in the selected group of patients with tumors that present a high grade of uptake of [111In] pentaoctreotide (octreoscan) scintigraphy.
Biological treatments with a promising prospect include sunitinib, everolimus and bevacizumab when associated with capecitabine and oxaliplatin.
MIBG Radiolabeled Therapy -
Some neuroendocrine tumors absorb a hormone called norepinephrine. These tumors may respond to a nuclear medicine technique called MIBG radiolabeled therapy. In this treatment, the patient is given an intravenous dose of MIBG, a protein that is similar to norepinephrine and is attached to a radioactive substance. The MIBG is absorbed by the tumor, permitting the radioactive substance to selectively destroy tumor cells.
PRRT is a molecular therapy used to treat NENs. In PRRT, a cell targeting protein (or peptide), similar to the natural circulating harmone somatostatine combined with a small amount of radio active material (yttrium or lutetium) tocreate a radio peptide. This radio peptide binds to neuroendicrine cells, delivering targeted high dose of radiation directely to the cancer cells.
Follow-up
Patients should be followed at 3-monthly intervals during treatment with cytotoxic agents or biological therapy in order to assess response to treatment. Patients undergoing curative surgery should be followed every 3-6 months for at least 5 years in order to detect eventual surgically removable recurrences. Examination should include specific or non-specific biochemical markers depending on the associated (or lack of) clinical syndrome. Imaging is based on CT or MRI every 6 months.